Best Practices for Maximizing your Electronic Health Records (EHR)
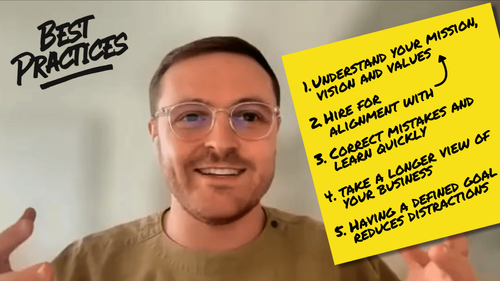
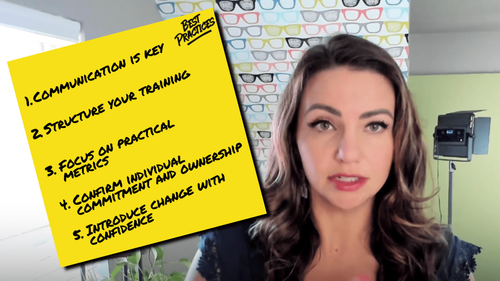
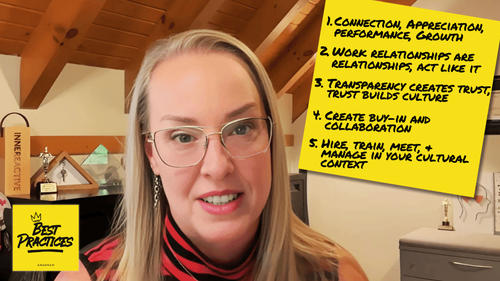
Listening to Steve Alexander’s conversation with Colton Calandrella on episode 11 of Best Practices made me rethink how we show up to the systems our practices rely on. We’re all guilty of using the basics, doing what keeps things moving, assuming the limitations we feel are baked into the software, not realizing how often those ceilings come from our own gaps in understanding.
And that’s the part that stuck with me: the space between where your EHR is today and where you want it to be is usually a matter of engagement, not capability. That gap in engagement is exactly what turns a powerful platform into a perceived limitation. The good news is that once you shift from “getting by” to intentionally learning the system, your EHR stops acting like a hurdle and starts operating like an advantage.
Check out the episode here:
Most Practices Aren’t Underperforming, They’re Underutilizing
The point that struck me first was how much capability sits untouched inside tools we already pay for. Colton described it perfectly: many teams live at the bare-minimum level of their EHR because that’s where they’ve always been, and when I heard that, I caught myself nodding. Think about it, continuing education is standard for clinical work but almost nonexistent for the systems that support it. When you build time to learn the software, the software becomes a catalyst rather than a ceiling
Leadership Sets the Pace
Another idea that landed hard for me was how powerful leadership modeling can be. Colton talked about the value in appointing an internal “EHR champion,” but it's important for leaders to understand that they can’t easily delegate proficiency they don’t have.
If owners and managers take the time to truly understand the system, it sends a message that it is part of what makes the practice run well. And when leaders demonstrate curiosity and competence, teams tend to rise with them, or at least begin to ask the right questions. Just as importantly, think of the inverse: what happens when leaders model poor PM System behavior?
This takeaway reinforced my belief that while people shape the culture, the way leaders use technology influences the standards that culture grows around.
Hiring for the Work You Actually Do
As the episode unpacked how much an EHR shapes the rhythm of a practice, it made me reconsider what “qualified” really means in a modern office, and technical adaptability has to be part of that definition. You need people who can grow with your systems, not just operate whatever they walked in knowing or skirting by learning the bare minimum.
If an EHR powers so much of your workflow, then bringing in people who struggle with technology is like building a house on a weak foundation. If you’re spending more time correcting or ignoring problems than you are building for the future, you should probably reevaluate your process.
The next time you interview a candidate, it’s worth evaluating their capacity to adapt, not just their experience. Making adaptability visible in the interview gives you a clearer sense of who can actually support the practice you’re building today, tomorrow, and into the future.
Turning Learning Into a Habit
I appreciated the constant emphasis throughout the episode on making EHR education continuous. It doesn’t need to be dramatic, but it compounds quickly. The irony is that EHR companies offer more training, office hours, webinars, and resources than most of us ever touch, so stay plugged into those support channels and stay ahead, it will help you stay in tune with what your tools can really do and align your ongoing EHR use with your practice goals.
In my mind, the icing on the cake is when practices build a feedback loop, both internally and externally. Internally, your team should be sharing what’s working, what’s confusing, and what could be better. Externally, your EHR provider should hear the same. When you treat your software provider like a partner instead of a vendor, you can both evolve together, as opposed to growing separately or even in spite of each other.
Where It All Landed For Me
What struck me after listening to this conversation is how much influence our EHR has on the tone and rhythm of our practice, long before we ever think about features or workflows. The way we engage with it, how we learn it, and how we weave it into our decisions quietly shapes the experience patients feel and the confidence our teams bring to their day. Once you see it in that light, the idea of “software management” feels far too small for what’s really at stake.
Because of that, I’ve started to think of EHR investment less as technical upkeep and more building the foundation that your practice runs on. A small, steady commitment to learning today becomes the reason patients move through your office smoothly tomorrow. It becomes the reason your team feels supported rather than frustrated. If a little EHR effort can help your practice feel less chaotic and more human, imagine what it could do for your bottom line.